Interview with Dr Meg Lewis
 Antidote Europe (AE): At what point in your science training did you begin to question the value of animal models with respect to human medicine? What are your current views on animal experiments in the field of research and testing and how did you come about them?
Antidote Europe (AE): At what point in your science training did you begin to question the value of animal models with respect to human medicine? What are your current views on animal experiments in the field of research and testing and how did you come about them?
Meg Lewis (ML):
It wasn’t until my current post that I became aware of the inefficacies of animal experiments, almost 4 years after I’d completed my PhD training.
The accepted thinking had always been that animal models are used where it would be unethical to do a test on a human – for example to find out if a compound is toxic. The motivation behind animal experiments is that they are supposed to give us information about whether something would be effective in humans, whether it would cause harm and to what extent. The underlying assumption is that animals are good models of humans, and that the information obtained from experimenting on them allows us to make accurate predictions of what happens in humans. I was shocked to learn the extent to which this is simply not the case.
We’ve known about the inefficacies of animal experiments for a long while, certainly since the 1960s, so I’m surprised that it hasn’t cropped up during my education. The figures are staggering – 94% of the drugs that make it past pre-clinical testing in animals fail at the clinical trials stage because they are either toxic or not effective in humans. There were an estimated 197,000 deaths related to adverse drug reactions in the EU in 2011. The increasing cost of getting a single drug to market (now an estimated average in the range of $1.5bn – $6bn), and the diminishing returns the pharmaceutical industry is seeing are bringing the sector into economic crisis. Animals are not humans, and respond differently to drugs. We need to accept these insufficiencies in current testing and move away from the use of animals for research and toxicology by developing in vitro tests and assays based on better science, that are more sensitive and more accurate than animal tests.
The replacement of animals in research and testing is not going to happen overnight, and may not even happen completely, but the earlier we start, and the more time and money we invest in alternative solutions, the more successful the end result will be.
AE: Today you are employed full-time as R&D Manager in a forward-looking biotech company (Kirkstall Ltd). Could you describe to our readers your proprietary product “Quasi-Vivo System” and what role it plays in the replacement of animals in research and testing?
ML:
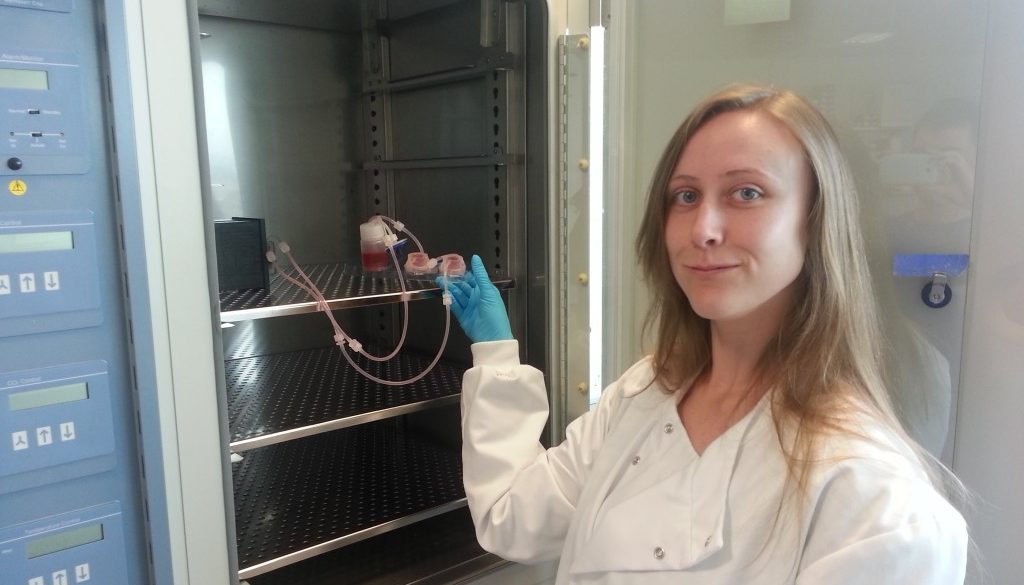
Kirkstall has a strong commitment to the 3Rs. The Quasi-Vivo system is a tool for cell culture, and can be thought of as a “Lego kit” for cell biologists, allowing them to culture cells in an environment which more closely represents the way that cells grow in the human body.
In order to successfully replicate the in vivo environment in vitro, a number of key in vivo aspects are required: the architecture of the organ and secreted factors that would be present in the extracellular matrix, tissue movement and plasticity, blood flow, specific oxygen pressures, and co-culture of the different cell types that make up an organ. The balance of these elements will depend on the requirements of each tissue, for example, bone cells will function best under higher pressures on a rigid 3D scaffold, and lung cells will prefer an environment under lower pressure with an air interface.
The central element of the Quasi-Vivo system is to expose cells to flow, with different chambers designed to support specific tissues in specific ways, by simulating their environment either through the chamber itself (as in our air-liquid interface chamber designed for skin or lung culture) or through compatibility with other technologies that replicate other key elements of the in vivo environment. Most standard cell culture is done in cell culture medium under static conditions. The introduction of a dynamic environment, where the medium is circulated by a pump and passes across cells, ensures cells are constantly provided with fresh nutrients, stimulated by low shear stress, and kept oxygenated. Recirculation of medium allows cells to condition their environment with secreted cytokines, as they would do in the body, increasing their longevity and proliferation, and enabling different tissues to talk to each other between chambers modelling inter-organ communication in vivo. This type of system makes it possible to look at how the drug metabolic products affect different organs without using an animal model.
Building a representative in vitro environment encourages cells to behave as they do in the body – we have had great success with our system in getting cells to function in similar ways to in vivo in terms of gene expression, drug metabolism, and improved longevity in culture. The system has been used to detect the toxicity of the drugs diclofenac, roflumilast and cyclophosphamide with between 4 and 30x greater sensitivity than standard in vitro assays.
AE: What advantages does your “Quasi-Vivo System” have over those of your competitors? Is there scope for improvement of your product or collaboration with like-minded scientists?
ML:
Groups developing technology in this area of bioscience are often doing so out of a drive to improve in vitro cell culture, and make it more representative so that data from in vitro experiments gives a more accurate picture of what is happening in the human in vivo environment. This has led to ingenious solutions for reducing and eventually replacing the need for animals in research, including spheroids to mimic 3D tissue strictures, and the ‘human on a chip’ idea of fluidic microchips where small populations of cells can communicate with each other through microscopic channels, in addition to our own system.
The Quasi-Vivo system is designed around the novel idea of individual chambers that can be interconnected to model the in vivo environment communications between organs in an easy-to-use way. The system enables researchers to study these communications and the effects they have on populations of cells without having to worry about technical problems such as leaks (which often plague other flow systems), bubbles and pressure artefacts (problems that come with microfluidics). The dimensions of the chambers are modelled on a standard 24 well plate commonly used for in vitro research, so they are compatible with 3D cell scaffolds designed for that size of culture vessel. Cells can be easily recovered after experiments, in numbers suitable for analysis of gene expression or protein levels.
We welcome any collaborations with like-minded scientists as we continue to develop our system for new applications. Our system is compatible with many other alternative technologies, such as induced pluripotent stem cells and 3D culture scaffolds. We believe that by working together with these technology providers we get the best out of the cells, and stand the best chance of making realistic in vitro models to replace animal use.
AE: How do you see the future of R&D in your field? If you had a budget of £ 10 million today, what would be your number one R&D priority?
ML:
The future is very bright, not only in the field of alternative technologies, where recognition and funding are increasing year on year, but also in the fields these technologies impact, such as general bioscience research, toxicology testing and so on. We know what the problems are, and we know the solutions, so it is just a matter of connecting the dots, developing these alternative technologies in synergy and optimising them to provide the most realistic models possible.
My research priorities for alternative technologies over the next 5-10 years would be to continue to develop and optimise new models and explore new applications, particularly where animal use is prevalent as in cancer research and toxicology testing. Alternative models will also be able to support the growing sphere of personalised medicine, which is reliant on individual human data, for example by providing a platform for testing a patient’s susceptibility to a drug for multiple organs in a connected system, using cells derived from a patient’s blood and then re-differentiated to lung, kidney, liver or heart. It will be very interesting to watch how the landscape develops.
AE: We thank you for giving up your time for this interview. Are there any additional comments that you would like to add that were not covered in the interview?
ML:
In my opinion, the long-term answer to widespread adoption of alternative technologies lies in education and in streamlining the alternative methods validation process.
If students could be taught about the pros and cons of animal testing and the availability of other solutions, they would come out of school or University with an informed, critical perspective on animal experiments, and this would encourage them to question and consider alternatives rather than re-enforcing the doctrine that animal experiments are necessary in order for developments in medicine and science to continue. Part of our aim as a company is to teach scientists the value of alternative technologies, and how to adopt them, in our monthly training courses.
Validation remains a significant roadblock to uptake of alternative methods by industry. At 10 years and €5m average investment to get a single assay validated by ECVAM, the cost is simply too great for most small companies, but without it, it is very difficult to convince contract research organisations and pharmaceuticals to use new technology and change their approaches (though not impossible).
CV:
Meg Lewis graduated from the University of Sheffield with a BSc in genetics and microbiology and a PhD in molecular biochemistry, after which she worked for the Department for Business, Innovation and Skills before joining Kirkstall in May 2011. As Principal Researcher, she oversaw the completion of the second TSB-funded Grant for Research and Development project, and had involvement in a number of commercial and collaborative projects.
In her current role as Research and Development Manager, she co-ordinates the research programme and research strategy, puts together new collaborative projects with leading research groups from across the world, and this year established a course programme training researchers how to use the Quasi-Vivo system.
In addition to research work, she is involved in supporting commercial relationships and academic partnerships in a technical and supervisory role, and in 2012 founded the Kirkstall Young Scientist Programme for science graduates in collaboration with the Job Centre to help new researchers into jobs in relevant fields.